Rushewar Patella shine a tsaye, a kwance ko ƙaura daga matsakaici na tibia (lambobin M21.0 da M22.1 bisa ga rabe-raben ICD-10). Tare da irin wannan rauni, mummunan ciwo nan da nan yakan faru, motsi na gwiwa ya toshe, aikin tallafi na ƙafa ya ɓata wani ɓangare ko gaba ɗaya. Tunda alamun sun yi kama da na karayar gwiwa, likita ne yake yin cikakken bincike ta hanyar amfani da x-rays. Bayan wannan, ana dawowa patella zuwa ga wurin kuma an ba da umarnin ci gaba - cikakken hanawar gaɓa na tsawon makonni uku zuwa wata ɗaya da rabi ko tiyata. Sai kawai a cikin 25% na lokuta irin wannan ɓarna yana faruwa ne sakamakon rauni, sauran kuma saboda rauni da jijiyoyi da rauni, lahani iri-iri na gwiwa ko haɗin mata.
Knee da patella ilmin jikin mutum
Ofayan manyan gabobin da ke samar da tafiya a tsaye, gudu da tsalle shine haɗin gwiwa. Yana da hadadden tsari kuma ya kunshi:
- Tibia, fibula da mace, patella (patella).
- Hanyoyi biyu na ciki da na ciki guda biyar.
- Jakuna biyar na synovial.
- Muscleungiyoyin tsoka guda uku (gaba, baya da na ciki).
An kirkiro patella ne daga ƙwayar cuta a lokacin haɓakar ɗan adam (kimanin shekaru bakwai). Yana da siffar dala ko kuma tetrahedral mai kusurwa uku tare da zagaye zagaye. Sashinta na ciki (tsaunin tsayayye wanda aka lulluɓe da guntun hyaline) yana a cikin ramin katako na femur. Gefen lebur yana fuskantar bayan haɗin gwiwa, kuma an haɗe shi daga ƙasa ta hanyar jijiyar kansa zuwa tibia, kuma daga sama zuwa jijiyoyin tsoka quadriceps na cinya. Alamar tana ba da kariya daga lalacewa kuma tana daidaita matsayin ɓangarorin haɗin gwiwa, kuma idan aka faɗaɗa shi, yana canzawa yadda ya kamata ƙarfin tsokokin cinya zuwa ƙananan ƙafa.

Ee Teeradej - stock.adobe.com
Irin
An rarraba raunin Patellar zuwa:
- Saboda abin da ya faru:
- tasirin tashin hankali na waje;
- na haihuwa ko wanda aka samu, sakamakon cutar, sauye-sauyen cututtukan cikin gwiwa.
- A cikin jagorancin ƙaura:
- a kaikaice;
- Rotary;
- a tsaye.
- Ta hanyar lalacewa:
- haske da matsakaici - ɗan canji kaɗan a cikin matsayin patella ba tare da fashewar jijiyoyin ba;
- m - rarrabuwa na farko, wanda yake tare da cikakken ƙaura na patella da lalata abubuwan da ke kewaye: guringuntsi, jijiyoyi;
- al'ada - maimaita sau da yawa saboda sauye-sauyen cututtukan yanayi, ɓarna ko subluxation.

© designua - stock.adobe.com
Dalilin
Yin wasan ƙwallon ƙafa, ɗaga sama, tsalle, tuntuɓar wasan tsere da sauran wasanni, waɗanda ke haɗuwa da huhu mai kaifi, faɗuwa, busawa zuwa gwiwa da ɗora nauyi a gwiwa a gwiwa, sau da yawa yakan haifar da raunin tashin hankali na patella da cututtukan cututtuka irin su jinkirtawa (matsuguni na dindindin zuwa gefen waje) da kuma osteochondropathy (canje-canje na degenerative a jikin guringuntsi).
Ragewa na iya faruwa saboda ci gaban mahaukaci ko rashin ci gaban abubuwan haɗin haɗin gwiwa. Tsoffin raunin gwiwa ko canje-canje masu lalacewa a tsarinta saboda rashin lafiya ko tiyata na iya haifar da rauni.
Kwayar cututtuka
A cikin lamura na farko, ciwo mara haƙuri koyaushe yakan tashi, ana jin haɗin gwiwa gwiwa yana yawo kuma an toshe motsinsa. A cikin mummunan rauni, cikakken fashewar jijiyoyin da lalata guringuntsi na iya faruwa.
Tare da rarrabuwa, patella gaba daya ya bar gadonta ya canza:
- Hagu zuwa dama ko hagu tare da rabuwa ta gefe - ana iya ganin ɓacin rai a tsakiyar gwiwa, kuma ana ganin tarin fuka mara kyau daga gefe.
- Kusa da tsaka-tsakin tsaye a cikin torsional dislocation - tsakiyar ɓangaren haɗin haɗin yana faɗaɗa ba bisa al'ada ba.
- Sama ko ƙasa tare da rarrabuwa a tsaye - bi da bi, patella tana da matsayi sama ko ƙasa da al'ada.
Yawancin lokaci, gwiwa yana ɗaukar matsayi na al'ada a kansa lokacin da aka miƙa ƙafa. Tsananin ciwo yana raguwa, edema ya bayyana. Ba a dawo da motsi na haɗin gwiwa ba kuma zubar da jini cikin rami yana yiwuwa. Dogaro da irin raunin, ciwo an gano shi a cikin yankin na medin retinaculum, na bayan femoral condyle, ko tsakiyar gefen patella.
Don kar a rikice rikicewa tare da karaya daga haɗin gwiwa, dole ne a bayyana ganewar asali ta amfani da X-ray.
Tare da subluxation, ciwo na ciwo mai sauƙi ne. Motsi na gwiwa kusan ba shi da iyaka, rabewar patella ya ɗan bambanta da na al'ada. Lokacin lankwasawa ko lankwasawa, ya bayyana: cushewa, jin bugowar ƙafa da rashin haɗin gwiwa.
Diagnostics
Tare da bayyanannun alamun rauni na rauni, patella ba zato ba tsammani ya faɗi a wuri ko likita yayi hakan yayin gwajin farko. Don bayyana yiwuwar lalacewa, ana ɗaukar rayukan haɗin gwiwa a cikin jirage biyu ko uku.
A yanayin rashin isassun bayanai na roentgenogram, ana yin lissafi ko yanayin yanayin maganaɗisu. Lokacin da ake zargin jini a cikin ramin patella, to ana amfani da huda. Idan ya zama dole don samun cikakken bayani game da yanayin abubuwan gwiwa, ana amfani da arthroscopy.
Idan canje-canjen cututtukan cututtukan da ba na tashin hankali ba suka zama sanadin wargazawar, to sai a ɗauki matakai don tabbatar da cutar da ta haifar da su, kuma ana yin nazarin ta sosai.
Taimako na farko
Da farko dai, ya kamata a cire ciwo na ciwo - ya kamata a yi amfani da damfara mai sanyi a gwiwa kuma a ba da cutar ga wanda aka azabtar. Sannan ya zama dole don tabbatar da rashin motsi na haɗin gwiwa ta amfani da duk wani abu da ake samu, bandeji na roba, bandeji na musamman ko tsaga. Ya kamata ku ba da lankwasa ƙafa mai lankwasa ko gyara ɓarna. Don kauce wa rikitarwa da bayyanar ɓarna na al'ada, ya zama dole a kai mara lafiya zuwa ɗakin gaggawa da sauri.
Wane likita za a tuntuɓi
Dogaro da nau'i da darajan lalacewa, ɓarkewar patella ya tsunduma cikin:
- Traumatologist - ganewar asali da magani.
- Likita - yin ayyukan.
- Orthopedist ko vertebrologist - gyarawa da sake dawowa.
Jiyya
Matsayin mai ƙa'ida, raguwar ɓarkewar ɓarkewa ta ƙwararren likita yana da sauri kuma yana da ɗan ciwo. Sannan aka ɗauki X-ray mai kulawa kuma, idan babu ƙarin lahani da aka gani, haɗin gwiwa yana motsawa tare da filastar filastar. Game da rashin neman taimakon likita (fiye da makonni uku bayan rauni) ko kuma a cikin mawuyacin yanayi (rabuwar al'ada, cikakken fashewar jijiyoyi, lalata guringuntsi), ana yin tiyata a buɗe ko arthroscopy.
Gyarawa, sharuɗɗan murmurewa da saka simintin gyaran kafa
Tsawon lokaci da nau'ikan abubuwan da suka faru bayan tashin hankali gaba ɗaya sun dogara ne da tsananin raunin da kuma hanyoyin magani. Lokacin haɓakawa zai iya kasancewa daga makonni uku zuwa watanni shida. Ofaya daga cikin hanyoyin da aka tsara da farko shine tausa mai warkewa, wanda wani lokacin ake fara amfani dashi a hankali ga tsokokin cinya da ƙananan ƙafa kai tsaye bayan kawar da ciwo da kumburi. Don dawo da sautin tsoka da motsi na gwiwa bayan cire filastar, ban da tausa, suna fara haɓaka haɗin gwiwa, da farko tare da taimakon likita, sannan kuma da kansu tare da taimakon motsa jiki na musamman.
Hanyoyi daban-daban na ilimin lissafi suna da tasiri mai amfani a kan hanyoyin dawo da laushi na jijiyoyi da sabunta tsokoki: UHF, electrophoresis, fitowar laser, aikace-aikacen esokerite.
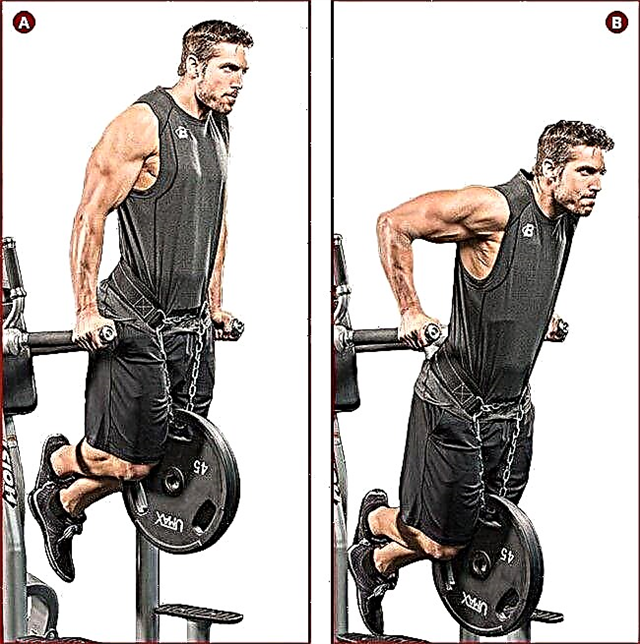
Magungunan jiki (maganin motsa jiki) an tsara shi makonni 2-3 bayan cire filastar. Da farko, tare da danniya kadan da karamin motsi. Don kauce wa maimaita patella da ke fitowa a wannan lokacin, ya zama dole a sa bandeji mai gyara. Bayan haka, a tsakanin watanni 2-3, nauyi da kewayon motsi suna ƙaruwa sannu a hankali. A ƙarshen zamani, an dawo da ikon yin tafiya tare da bandeji mai tallafi. Don kar a sake rarraba patella a yayin yin motsa jiki na jiki wanda baya ware faduwa, ya zama dole ayi amfani da takalmin gwiwa. Cikakken dawo da haƙurin motsa jiki da ikon gudu da tsalle ana samun shi ta hanyar manyan atisaye a cikin wasan motsa jiki na likitanci tsawon watanni 6-12.
Sakamakon da lalacewar jingina
Rushewar patella na iya rikitarwa ta mummunar lalacewar jijiyoyin da ke kewaye, guringuntsi, manisci. Rashin tuntuɓar likita ko ragin da bai dace ba na iya haifar da rabuwar al'ada da kuma saurin yin gwiwa. A cikin mawuyacin yanayi, musamman bayan tiyata, kumburi da jijiyoyin jijiyoyin jikin mutum ko kuma rufin mahaɗan mahaifa na iya faruwa.